In a previous blog post, we discussed how we shouldn’t waste our time worrying about posture (even though many people believe it is key for back health – it is not).
So, what can we do about pain? What should we put our time and energy into if posture doesn’t matter? We will explore some factors that, according to scientific research, truly do matter – but first a word on the incredible adaptability of the body.
Runners’ Youthful Knees, Hips and Backs:

Runners are less likely to develop hip and knee osteoarthritis (OA) when compared to others who do not meet their weekly exercise recommendations (1). You read that correctly – runners are LESS likely to develop arthritis in their hips and knees. They even have healthier, more youthful appearing discs in their backs (2). As do cyclists (3). And weightlifters have stronger thicker cartilage in their knee joints, as well as stronger ligaments and tendons (4, 5, 6).
So, runners, who subject their knees, hips and spines to multiple times their bodyweight with every stride they take (7, 8) have healthier joints and spines. And cyclists, who sit bent over for hours on end during rides, have spinal discs that appear healthier. This may not make sense to some people, but it does when you consider that the body is adaptable – that it will respond and adapt to the stresses and strains that we subject it to.
Now, there is some evidence that marathoners develop more knee and hip arthritis than runners who don’t run such excessive distances, but this is still up for debate and research continues in this area (1). Some researchers have even found lower rates of arthritis in marathoners compared to the general population (9). The higher rates of osteoarthritis in marathoners (when compared to runners who cover less ground) might suggest that excessive loads, over-training or pushing through injuries consistently might increase the risk of issues in the joints down the line. There is, undoubtedly, a limit to what our bodies can tolerate (which is different for each person – depending on genetics, experience and lifestyle factors).
“You Are Not Machines... You Are Men (and Women)!”
Charlie Chaplin’s spine-tingling speech from ‘The Dictator’ comes to mind when we talk about adaptability. During this inspiring speech he tells us that we are not machines. And he is right. Unlike machines, we do not wear down a little bit more with each use. We are alive. We adapt, change, grow and become more resilient.
If runners’, cyclists’ and weightlifters’ bodies and joints remain healthy into later life compared to the rest of us, despite them subjecting themselves to regular and repetitive heavy loads, then we need to reassess how we view the body. The term ‘wear & tear’ needs to be thrown out.
Back to Pain – What Matters?
It might come as no surprise, based on what you have just read above, that being active and meeting your exercise guidelines is associated with less suffering with pain (10) (for more on this, read this previous blog post).
For those who claim to be allergic to exerting themselves, you will be happy to hear that another activity that can help with pain involves as little effort as possible.
Sleep

Sleep is essential for health and is absolutely linked to pain – including the risk of pain becoming more persistent (11). It is also linked to many other health issues – like cardiovascular disease, mental health problems and neurological conditions (12).
When you consider what we do while we sleep, it actually brings to light how important it really is. Consider the fact that we are helpless and vulnerable while we sleep. We are also completely unproductive (at least on the surface) while we sleep. Yet we still spend 1/3rd of our lives asleep (7-9hrs per adult is essential for health – depending on individual factors).
Consider that our ancestors had to survive over 250,000 years on this planet, 1/3rd of this time they spent asleep. If sleep wasn’t important, it would quickly have been removed from the picture by the forces of evolution – with those humans requiring less sleep surviving and thriving due to more productive hours each day and less time spent in vulnerable sleep. The fact that this didn’t happen, and we still need 7-9hrs of sleep for optimum health shows that clearly something very important goes on while we sleep.
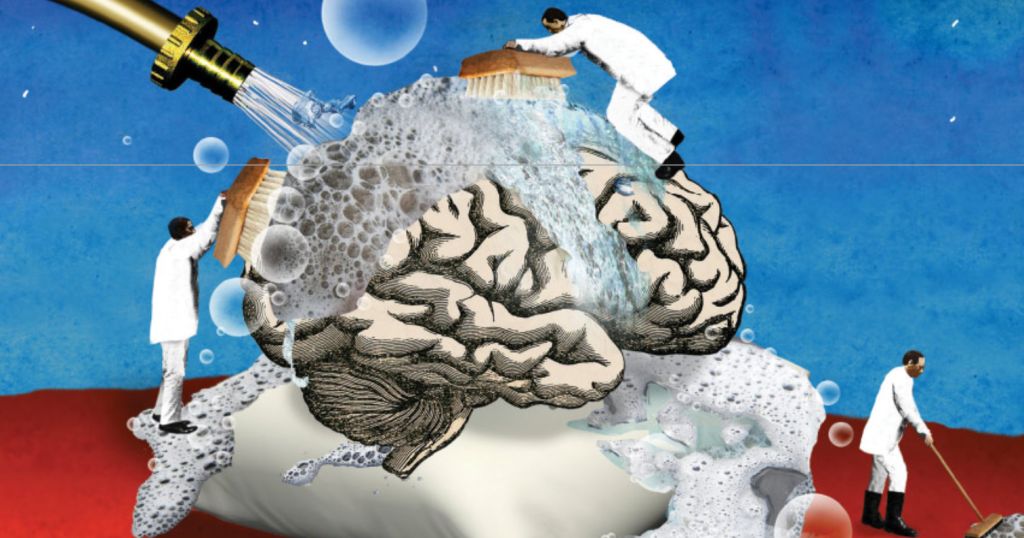
And it does. Sleep is essential for all aspects of health and wellbeing. During sleep we clear waste products from the brain that build up during the day and restore the brain’s chemical balance. Proteins called ‘amyloid plaques’, prominent in those with dementia and Parkinson’s, are less common in those who get adequate sleep (13). Sleep is essential for learning and memory formation. Our immune system depends on sleep – with good sleepers less likely to suffer from infections and able to develop immunity more effectively. Wounds even heal better when we have a good night’s sleep (13).
As mentioned earlier, sleep is a key factor in helping to reduce suffering with pain. Good quality sleep is associated with less injuries – with young athletes twice as likely to get injured if they don’t get adequate sleep (14). This trend continues into adulthood – with significantly more injuries taking place in workplaces the week following daylight savings (when people tend to lose an hour of sleep) (15).
So, take all that thought and effort that you put into your posture and direct it towards your sleep.
Connection & Loneliness Affects Our Health

How connected we are and feel has a strong impact on our health and wellbeing. Leading researchers have been able to show that loneliness can be as damaging to health as smoking 15 cigarettes a day or being obese (16). Loneliness is also associated with cardiovascular health, mental health and cognitive decline in older age (17, 18). Loneliness has a strong connection with pain – with lonely people more likely to suffer from pain issues in the future, as well as being more susceptible to pain becoming persistent (19).
It may not be a surprise that loneliness affects our mental health, but how can loneliness, a subjective feeling, be linked with our physical health? Loneliness literally causes changes in many key systems within the body – including our nervous system, immune system, endocrine (hormones) system and cardiovascular system (17, 18). Researchers have been able to measure chemical and hormonal changes that take place within the body in response to loneliness, with long-term loneliness being associated with structural changes in the brain and heart (17, 18).
From an evolutionary perspective it appears that we are primed to be social. Our ancestors would never have survived alone. They evolved within groups – supporting and being supported in equal measure. This seems to have seeped into our DNA, become a part of who we are – it’s like we have a biological drive to connect and support (20). This is reflected in the health benefits of connection and support, and the detrimental effects of not having these things.
Loneliness is a subjective experience, with different people needing different amounts and depths of social interactions to feel socially fulfilled (17, 18).
The List Goes On...

When people think about preventing injuries and pain, often their minds go to physical interventions. However, the body works the way the body works. We are biological organisms, and we are affected by literally everything in our environment to greater or lesser degrees. Consider how plants depend on a wide range of conditions for their health (such as sunlight exposure, minerals, water, shade, shelter, safety from predators, etc etc etc).
When it comes to pain, there is a long list of factors that play a role – amongst them; stress, obesity, diet, mood, beliefs (e.g. fear of pain and avoidance behaviours) (21). Even childhood experiences can play a role – with those subjected to traumatic experiences, neglect and different forms of abuse more likely to suffer from pain and other health issues in adulthood (22).
Each Small Step Is Powerful

As always, the following is general advice and is for educational purposes. Every individual is different, and if required it is always best to seek individualised advice and guidance.
Exercise:
- Meet your weekly exercise recommendations as often as possible. For more on this, read this blog post.
Sleep
- Read up on sleep hygiene and take some steps to improve your sleep habits.
- Insomnia – Psychologists provide the ‘gold standard’ treatment. Don’t just go for quick fixes like sleeping tablets.
Connection/ Loneliness:
- Aim to spend time with those you feel yourself around
- Join a club/ community with shared interests
- Seek help and support if needed
We can’t do this alone
We should all aim to meet our individual requirements for individual health and wellbeing. However, we are part of larger groups, as well as a wider society and culture that affects us and everyone around us.
As a society we should strive for access to quality healthcare and education, as well as leisure facilities and outdoor spaces. We all should be able to engage in meaningful activities. Equality of opportunity is essential – if there are people in our societies that miss out on any of these opportunities, we must take action to address it immediately.
Considering all that you have just read (and well done for making it this far!), making positive changes in any one of these areas will have a knock-on effect, a positive spill, into many other aspects of health and wellbeing. This is the beauty here – small, consistent changes made to help with something like pain will have a beneficial effect on many other aspects of health.
We are adaptable, we are shaped by what we do regularly. So, consistency is key. Acknowledge that changing ingrained habits is challenging, takes time, often involves setbacks and takes conscious effort (at least in the early days). But know that it becomes much easier with time and practice.
Useful Resources:
References:
- Alentorn-Geli E, Samuelsson K, Musahl V, Green CL, Bhandari M, Karlsson J. The Association of Recreational and Competitive Running With Hip and Knee Osteoarthritis: A Systematic Review and Meta-analysis. J Orthop Sports Phys Ther. 2017 Jun;47(6):373-390. doi: 10.2519/jospt.2017.7137. Epub 2017 May 13. PMID: 28504066.
- Belavý, D.L., Quittner, M.J., Ridgers, N., Ling, Y., Connell, D. and Rantalainen, T., 2017. Running exercise strengthens the intervertebral disc. Scientific Reports, 7(1), pp.1-8.
- Belavy, D.L., Quittner, M., Ridgers, N.D., Ling, Y., Connell, D., Trudel, G. and Rantalainen, T., 2019. Beneficial intervertebral disc and muscle adaptations in high-volume road cyclists. Medicine and science in sports and exercise, 51(1).
- Grzelak, P., Podgorski, M., Stefanczyk, L., Krochmalski, M. and Domzalski, M., 2012. Hypertrophied cruciate ligament in high performance weightlifters observed in magnetic resonance imaging. International orthopaedics, 36(8), pp.1715-1719.
- Grzelak, Piotr & Polguj, Michał & Podgórski, Michał & Majos, Agata & Krochmalski, Marek & Domzalski, Marcin. (2012). Patellar ligament hypertrophy evaluated by magnetic resonance imaging in a group of professional weightlifters. Folia morphologica. 71. 240-4.
- Grzelak P, Domzalski M, Majos A, Podgórski M, Stefanczyk L, Krochmalski M, Polguj M. Thickening of the knee joint cartilage in elite weightlifters as a potential adaptation mechanism. Clin Anat. 2014 Sep;27(6):920-8. doi: 10.1002/ca.22393. Epub 2014 Mar 20. PMID: 24648385.
- Bergmann, G., Deuretzbacher, G., Heller, M., Graichen, F., Rohlmann, A., Strauss, J. and Duda, G.N., 2001. Hip contact forces and gait patterns from routine activities. Journal of biomechanics, 34(7), pp.859-871.
- Schäfer, R., Trompeter, K., Fett, D., Heinrich, K., Funken, J., Willwacher, S., Brüggemann, G.P. and Platen, P., 2023. The mechanical loading of the spine in physical activities. European Spine Journal, pp.1-11.
- Ponzio, D.Y., Syed, U.A.M., Purcell, K., Cooper, A.M., Maltenfort, M., Shaner, J. and Chen, A.F., 2018. Low prevalence of hip and knee arthritis in active marathon runners. JBJS, 100(2), pp.131-137.
- Shiri, R. and Falah-Hassani, K., 2017. Does leisure time physical activity protect against low back pain? Systematic review and meta-analysis of 36 prospective cohort studies. British journal of sports medicine, 51(19), pp.1410-1418.
- Finan, P.H., Goodin, B.R. and Smith, M.T., 2013. The association of sleep and pain: an update and a path forward. The journal of pain, 14(12), pp.1539-1552.
- Grandner, M.A., Jackson, N.J., Pak, V.M. and Gehrman, P.R., 2012. Sleep disturbance is associated with cardiovascular and metabolic disorders. Journal of sleep research, 21(4), pp.427-433.
- Besedovsky, L., Lange, T. and Haack, M., 2019. The sleep-immune crosstalk in health and disease. Physiological reviews.
- Milewski, Matthew D. MD*; Skaggs, David L. MD, MMM†; Bishop, Gregory A. MS‡; Pace, J. Lee MD†; Ibrahim, David A. MD†; Wren, Tishya A.L. PhD†; Barzdukas, Audrius MEd‡ Chronic Lack of Sleep is Associated With Increased Sports Injuries in Adolescent Athletes, Journal of Pediatric Orthopaedics: March 2014 – Volume 34 – Issue 2 – p 129-133 doi: 10.1097/BPO.0000000000000151
- Barnes, C.M. and Wagner, D.T., 2009. Changing to daylight saving time cuts into sleep and increases workplace injuries. Journal of applied psychology, 94(5), p.1305.
- Holt-Lunstad, J., Smith, T.B. and Layton, J.B., 2010. Social relationships and mortality risk: a meta-analytic review. PLoS medicine, 7(7), p.e1000316.
- Haslam, C., Cruwys, T., Haslam, S.A. and Jetten, J., 2015. Social connectedness and health. Encyclopedia of geropsychology, 46(1), pp.1-10.
- Holt-Lunstad, J., Smith, T.B., Baker, M., Harris, T. and Stephenson, D., 2015. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspectives on psychological science, 10(2), pp.227-237.
- Loeffler, A. and Steptoe, A., 2021. Bidirectional longitudinal associations between loneliness and pain, and the role of inflammation. Pain, 162(3), p.930.
- Cacioppo, J.T., Cacioppo, S. and Boomsma, D.I., 2014. Evolutionary mechanisms for loneliness. Cognition & emotion, 28(1), pp.3-21.
- Mosley, G.L. and Butler, D.S., 2017. Explain pain supercharged. NOI.
- Hanlon, P., McCallum, M., Jani, B.D., McQueenie, R., Lee, D. and Mair, F.S., 2020. Association between childhood maltreatment and the prevalence and complexity of multimorbidity: A cross-sectional analysis of 157,357 UK Biobank participants. Journal of comorbidity, 10, p.2235042X10944344.

